Your cart is currently empty!
Historically, humans have battled with numerous infectious disease outbreaks. What lessons have we learnt to prepare for the current COVID-19 pandemic?
Here, we cover 3 of the deadliest pandemics that each shaped the world and revolutionised modern medicine.
Top twenty pandemics ranked based on death toll
| Rank | Name | Period | Cause | Death toll |
|---|---|---|---|---|
| 1 | Smallpox | 1157 BC- 1977 | Variola major virus | 360 million |
| 2 | Black Death | 1347-1351 | Yersinia pestis bacteria / Rats, fleas | 200 million |
| 3 | Spanish Flu | 1918-1919 | H1N1 virus/pigs | 40-50 million |
| 4 | Plague of Justinian | 541-542 | Yersinia pestis bacteria / Rats, fleas | 30-50 million |
| 5 | HIV/AIDS | 1976-present | Virus / Chimpanzees | 25-35 million |
| 6 | Third Plague | 1885 | Yersinia pestis bacteria / Rats, fleas | 12 million |
| 7 | Antonine Plague | 165-180 | Suspected smallpox or measles | 5 million |
| 8 | Asian Flu | 1957-1958 | H2N2 virus | 1.1 million |
| 9 | Cholera Pandemics 1-6 | 1817-1923 | V. cholerae bacteria | 1+ million |
| 10 | Japanese smallpox epidemic | 735-737 | Variola major virus | 1 million |
| 11 | Italian plague | 1629-1631 | Yersinia pestis bacteria / Rats, fleas | 1 million |
| 12 | Russian Flu | 1889-1890 | Suspected H2N2 (avian origin) | 1 million |
| 13 | Hong Kong Flu | 1968-1970 | H3N2 virus | 1 million |
| 14 | Swine Flu | 2009-2010 | H1N1 virus / Pigs | 200,000 |
| 15 | COVID-19 | 2019-Present | SARS-2 coronavirus | 177,200 |
| 16 | Yellow Fever | Late 1800s | Virus / Mosquitoes | 100,000-150,000 |
| 17 | Great Plague of London | 1665 | Yersinia pestis bacteria / Rats, fleas | 100,000 |
| 18 | Ebola | 2014-2016 | Ebolavirus / Wild animals | 11,000 |
| 19 | MERS | 2015-Present | Coronavirus / Bats, camels | 850 |
| 20 | SARS | 2002-2003 | Coronavirus / Bats, Civets | 774 |
Smallpox Pandemic (1157 BC – 1977)
Smallpox is a highly contagious disease caused by the variola virus, which killed about 360 million people globally between 1157 BC and 1977.
The first vaccine
But the fight against smallpox also gave the world the first vaccine, which was developed in 1796. English doctor Edward Jenner showed that exposing people to the cowpox – a milder virus form – could protect them against smallpox.
Following this landmark discovery, smallpox was globally eradicated by 1980. According to the World Health Organisation (WHO), the last naturally occurring case of smallpox occurred in 1977.

The Black Death (1347-1351)
The Black Death (Bubonic plaque) wiped out about 200 million people and killed over 50% of Europe’s population in the 14th century. It was caused by Yersinia pestis, a type of bacteria carried by rats and fleas before transmitted to people.
The Black Death was one of the first of a wave of plagues that swept across the world. In fact, the Italian plague and the Great Plague of London killed hundreds to millions more well into the 1700s.

Transformation of medicine and public health
When the Black Death struck in the 14th century, nobody knew how to prevent or treat the disease.
Some people fled or turned to “plague tractates”, essays often written by unlicensed “physicians”, to find answers. Others stayed and sought healing through prayers. Some lives were saved as a result of autopsies or surgeries to study the dead bodies of plague victims.
The outcomes to these approaches to curing the plague triggered drastic modifications to healthcare systems that revolutionised the field of medicine that we know and practice today:
- Medicine is now based on practical, empirical evidence rather than unproven theoretical predictions and propositions
- Strict regulations for medical professionals became mandated and unlicensed practitioners were forbidden from treating patients and
- The study of the human body such as surgery and anatomy were incorporated in the medical curriculum of all universities
The plague still exists in certain parts of the world. Antibiotics such as streptomycin, and doxycycline are the method of choice to treat it. However, there is still no commercially available vaccine.
Spanish Flu (1918-1919)
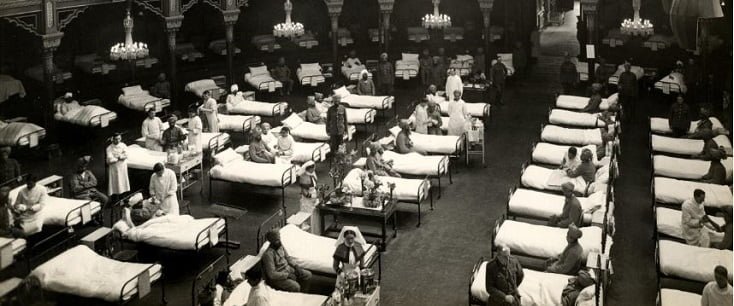
The Spanish flu pandemic erupted in 1918-1919, infected up to 500 million and killed about 50 million people. This airborne disease rapidly spread among healthy young adults during World War I. In fact, more solders died of the flu than they were killed in battle.
It came in two waves. The first wave had a low death toll and started in spring of 1918. But the second wave was far more deadly and followed in autumn and winter of that same year.

Introduction of public control measures
There were no effective drugs or vaccines to treat this killer flu. Officials pursued several public measures to stop the spread of the virus, including:
- Imposed quarantines
- Ordered citizens to wear masks
- Shut down festivities, public places, including schools, churches, and theaters
- People were advised to avoid shaking hands and to stay indoors
- Regulations were passed banning spitting
Sound familiar?
By the summer of 1919, the flu pandemic came to an end, as those that were infected either died or developed immunity.
COVID-19
Fast forward by 100 years and we have COVID-19. This viral respiratory syndrome spread to 210 countries globally and, to date, infected over 2.6 million and caused 184,217 deaths.
Officials are pursuing similar measures to the Spanish Flu like quarantines, closure of public venues, and social distancing. Moreover, they added the early closure of state and international borders.
What lessons can we learn from past pandemics to prevent and stop COVID-19 today?
- Prevention is the best cure. Continuous vaccine research and development is vital
- Treatments should only be implemented after being studied such as in clinical trials
- Sources of contagion should be removed to minimise spread from animals to humans
- Prompt response from the authorities is pivotal to contain the widespread of disease
- We need a national pandemic or crisis readiness action plan
Sources:
- https://www.history.com/news/the-rise-and-fall-of-smallpox
- https://www.who.int/csr/disease/smallpox/en/
- https://www.cdc.gov/smallpox/
- https://www.history.com/topics/world-war-i/1918-flu-pandemic
- https://www.cdc.gov/flu/about/qa/1918flupandemic.htm
- https://www.worldometers.info/coronavirus/